2. 分子心血管学教育部重点实验室,北京 100191;
3. 北京大学第三医院临床流行病学研究中心,北京 100191
2. Key Laboratory of Molecular Cardiovascular Sciences, Ministry of Education, Beijing 100191, China;
3. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
心血管药物中毒已经成为全球性的公共卫生问题[1]。钙通道阻滞剂(calcium channel blockers,CCBs)是一种临床常用的心血管药物,主要应用于治疗高血压,还可用于治疗冠状动脉性疾病和心律失常。CCBs临床需要量大且容易获得,近年来已成为导致中毒的常见心血管药物类型。不仅如此,严重的CCBs中毒导致死亡的占比正在逐年增加,2019年美国中毒控制中心报道因中毒导致死亡的病例中CCBs中毒占4.62%[2],而2020年报道比例已增至6.4%[3]。其造成死亡的病理生理基础是难以纠正的休克、循环系统的崩溃和致命的心脏骤停。
根据最新的国际专家共识,成人CCBs中毒的一线治疗包括补液、静脉钙剂、血管活性药物(去甲肾上腺素、肾上腺素或多巴酚丁胺)、大剂量胰岛素和阿托品。在难治性休克、围心脏骤停期和心脏骤停时,可使用静脉脂肪乳、起搏器或静脉-动脉体外膜肺氧合(veno-arterial extracorporeal membrane oxygenation, VA-ECMO)[4],其核心的治疗理念在于纠正休克或循环衰竭。
氨氯地平是最常见的二氢吡啶类CCBs,过去十年应用氨氯地平治疗高血压的患者增加了3倍[5]。在钙通道阻滞剂中,氨氯地平是报道最多的导致急性中毒的CCBs药物,也是造成死亡最多的CCBs药物[3]。目前有关氨氯地平中毒的临床研究较少,且多为个案报道,更未见氨氯地平中毒剂量与临床结果之间的相关性研究,为此在本研究中笔者回顾分析了因氨氯地平中毒并发休克而在北京大学第三医院急诊科救治的成年患者的病例资料并检索了已发表的氨氯地平中毒各类病例报道和临床研究,试图发现服药剂量与临床严重程度的关系,特别是与休克严重程度的相关关系,为预测和评估此类中毒的严重程度提供参考。
1 资料与方法 1.1 伦理审核本研究经北京大学第三医院医学科学研究伦理委员会审批,批号:(2022)医伦审第(292-02)号,免除知情同意获准。
1.2 研究对象回顾性选取因氨氯地平中毒并发休克在北京大学第三医院急诊科救治的成年患者,同时也检索了已发表的氨氯地平中毒个案、系列报道和临床研究中的成年患者。
纳入标准:⑴年龄≥16岁;⑵有明确的过量服用氨氯地平的病史或血药浓度提示氨氯地平浓度超出参考治疗剂量范围;⑶有休克的临床表现;⑷有服药剂量记录。排除标准:个案报道、系列报道和临床研究中的非英文文献。
1.3 数据检索以“Amlodipine overdose”“Amlodipine poisoning”“Amlodipine intoxication”为检索词在PubMed、Web of Science、和EMBASE上进行检索,研究类型为个案报道、病例系列报道和临床研究。检索1997—2022年的文献。
本中心病例资料来自北医三院的HIS数据库,检索了2018年1月1日至2022年12月31日的数据,以中毒或药物过量为主要诊断,筛选氨氯地平中毒并发休克的病例并纳入本研究。
1.4 资料收集收集性别、年龄、服药剂量、服药至就诊间隔时间、合并中毒物质种类及剂量、主要临床表现(如心脏骤停等)、既往史、接诊生命体征、主要治疗方法(如静脉钙剂、大剂量胰岛素、血管活性药物种类、静脉脂肪乳、心肺复苏等)、器官功能支持疗法(如机械通气、血液净化、ECMO等)、临床结局(生存至出院或死亡)、住院天数等指标。若计量资料无准确数值,为数值范围,则选用范围中间值进行分析。分组:根据病程中最差临床表现分成非难治性休克、难治性休克两组。休克定义为:收缩压<90 mmHg(1 mmHg=0.133 kPa),平均动脉压<65 mmHg,或循环支持需要≥2种血管升压药[6]。非难治性休克定义为通过一线治疗能纠正的休克。难治性休克定义为尽管一线治疗的基础上增加了正性肌力药物或血管加压药物的剂量,但休克仍持续存在[7],需要使用静脉脂肪乳、起搏器、左心室辅助、主动脉内球囊反搏或V-A ECMO等治疗。心脏骤停指积极治疗过程中突发心搏呼吸停止,并使用心肺复苏术。
1.5 统计学方法采用R 4.0.3(https://www.r-project.org/)统计软件进行数据处理。正态分布的计量资料以均值±标准差(x±s)表示,两组间均值比较采用独立样本t检验,非正态分布的计量资料以中位数(四分位数)[M(Q1, Q3)]表示,两组间比较采用Mann-Whitney U检验;计数资料以频数和百分数表示,组间比较采用Pearson卡方检验或Fisher精确概率检验。剂量与难治性休克间的关系采用受试者工作特征曲线(ROC)观察剂量诊断难治性休克的效能,并应用约登指数最大原则选取界值。所有假设检验当双侧P<0.05时认为差异具有统计学意义。
2 结果 2.1 基本资料本研究纳入共68篇病例报道和病例系列报道,1篇临床研究,其中包含患者74例,见表 1。纳入北京大学第三医院就诊患者6例。本研究最终共纳入80例患者。按照分组原则,表现为非难治性休克的患者37例,难治性休克43例,基本资料和接诊生命体征见表 2,治疗方法和临床结局见表 3。
| 文献作者 | 性别 | 年龄(岁) | 氨氯地平服药剂量(mg) | 仅氨氯地平中毒 |
| Bringgold等[8] | 女 | 39 | 300 | 否 |
| Patel等[9] | 女 | 24 | 500 | 否 |
| Tale等[10] | 男 | 66 | 125 | 否 |
| Matsushime等[11] | 女 | 54 | 345 | 否 |
| Hedaiaty等[12] | 女 | 36 | 500 | 是 |
| Reuter-Rice等[13] | 女 | 16 | 400 | 是 |
| Koliastasis等[14] | 女 | 72 | 200 | 是 |
| Hong等[15] | 250 | 否 | ||
| Hong等[15] | 女 | 350 | 否 | |
| Meaney等[16] | 女 | 47 | 350 | 否 |
| Gutierrez等[17] | 男 | 57 | 200 | 否 |
| Sandeep等[18] | 女 | 35 | 1 000 | 否 |
| Nordmark Grass等[19] | 女 | 28 | 1 000 | 否 |
| Upreti等[20] | 女 | 28 | 250 | 是 |
| Kumar等[21] | 女 | 22 | 900 | 是 |
| Ebihara等[22] | 女 | 81 | 250 | 是 |
| Kute等[23] | 女 | 28 | 250 | 是 |
| Chudow等[24] | 男 | 53 | 800 | 是 |
| Karbek Akarca等[25] | 女 | 25 | 100 | 是 |
| Brunette-Lawrey等[26] | 女 | 54 | 200 | 否 |
| Nasa等[27] | 男 | 69 | 50 | 否 |
| Ando等[28] | 男 | 73 | 420 | 否 |
| Gérard等[29] | 女 | 58 | 480 | 否 |
| Lai等[30] | 女 | 28 | 420 | 是 |
| Ramanathan等[31] | 男 | 25 | 550 | 否 |
| Weinberg等[32] | 男 | 50 | 500 | 否 |
| Naha等[33] | 女 | 18 | 85 | 否 |
| Ghosh等[34] | 女 | 25 | 100 | 否 |
| Ghosh等[34] | 男 | 65 | 50 | 否 |
| Gautam等[35] | 男 | 25 | 100 | 否 |
| St-Onge等[36] | 男 | 68 | 300 | 否 |
| Rizvi等[37] | 女 | 24 | 280 | 是 |
| Plumb等[38] | 女 | 50 | 770 | 否 |
| Kao等[39] | 女 | 49 | 150 | 否 |
| West等[40] | 女 | 71 | 135 | 是 |
| Agarwal等[41] | 男 | 51 | 500 | 是 |
| Harris等[42] | 女 | 40 | 1 000 | 是 |
| Haughey等[43] | 男 | 47 | 400 | 否 |
| Sutar等[44] | 女 | 28 | 400 | 是 |
| Wood等[45] | 男 | 43 | 560 | 否 |
| Jang等[46] | 女 | 25 | 400 | 是 |
| Beavers等[47] | 女 | 59 | 200 | 否 |
| Adams等[48] | 男 | 76 | 100 | 是 |
| Hopkins等[49] | 女 | 21 | 280 | 否 |
| Rasmussen等[50] | 女 | 36 | 280 | 否 |
| Zahed等[51] | 男 | 25 | 450 | 是 |
| Hung等[52] | 女 | 40 | 30 | 是 |
| El Houari等[53] | 女 | 27 | 150 | 是 |
| Essink等[54] | 女 | 17 | 525 | 否 |
| Osman等[55] | 女 | 73 | 400 | 是 |
| Azendour等[56] | 女 | 20 | 420 | 是 |
| Vogt等[57] | 男 | 42 | 1 000 | 否 |
| Connor-Schuler等[58] | 男 | 47 | 145 | 是 |
| Connor-Schuler等[58] | 女 | 39 | 600 | 否 |
| Hasson等[59] | 女 | 22 | 280 | 是 |
| Garg等[60] | 男 | 42 | 500 | 是 |
| Khan等[61] | 男 | 57 | 300 | 是 |
| Ezidiegwu等[62] | 女 | 22 | 425 | 是 |
| Laes等[63] | 男 | 61 | 200 | 否 |
| Varpula等[64] | 男 | 38 | 630 | 否 |
| Jović-Stosić等[65] | 女 | 24 | 150 | 否 |
| Kanagarajan等[66] | 女 | 22 | 800 | 是 |
| Shetty等[67] | 女 | 31 | 200 | 是 |
| Wilffert等[68] | 女 | 47 | 200 | 否 |
| Koch等[69] | 女 | 63 | 70 | 否 |
| Beyls等[7] | 男 | 61 | 450 | 否 |
| Beyls等[7] | 男 | 70 | 200 | 否 |
| Beyls等[7] | 男 | 50 | 900 | 否 |
| Miranda等[70] | 男 | 18 | 150 | 否 |
| Teker等[71] | 女 | 16 | 500 | 是 |
| Raj等[72] | 女 | 18 | 150 | 是 |
| Boyer等[73] | 女 | 34 | 30 | 是 |
| Saravu等[74] | 男 | 20 | 400 | 是 |
| Rafeq等[75] | 女 | 73 | 70 | 否 |
| 项目 | n1 | 非难治性休克(n=37) | n2 | 难治性休克(n=43) | 统计值 | P值 |
| 性别(%) | 37 | 42 | 4.354 | 0.037 | ||
| 男 | 10 (27.0) | 21 (50.0) | ||||
| 女 | 27 (73.0) | 21 (50.0) | ||||
| 年龄 | 37 | 35 (25, 54) | 41 | 47 (26, 57) | -0.976 | 0.329 |
| 服药剂量(mg) | 37 | 200(100.0, 300.0) | 43 | 400 (225.0, 537.5) | -3.421 | 0.001 |
| 服药至就诊间隔时间(h) | 31 | 6 (4.0, 8.0) | 27 | 5 (2.3, 9.7) | 0.851 | 0.395 |
| 是否合并其他中毒(%) | 37 | 43 | 2.207 | 0.137 | ||
| 否 | 19 (51.4) | 15 (34.9) | ||||
| 是 | 18 (48.7) | 28 (65.1) | ||||
| 同时服用其他CCB(%) | 37 | 43 | - | 1.000 | ||
| 是 | 0 (0) | 1 (2.3) | ||||
| 否 | 37 (100) | 42 (97.7) | ||||
| 同时服用β受体阻滞剂(%) | 37 | 43 | 0 | 1.000 | ||
| 是 | 5 (13.5) | 5 (11.6) | ||||
| 否 | 32 (86.5) | 38 (88.4) | ||||
| 同时服用ACEI(%) | 37 | 43 | 3.57 | 0.059 | ||
| 是 | 1 (2.7) | 8 (18.6) | ||||
| 否 | 36 (97.3) | 35 (81.4) | ||||
| 同时服用ARB (%) | 37 | 43 | 0 | 1.000 | ||
| 是 | 4 (10.8) | 5 (11.6) | ||||
| 否 | 33 (89.2) | 38 (88.4) | ||||
| 同时服用利尿剂(%) | 37 | 43 | 0 | 1.000 | ||
| 是 | 2 (5.4) | 2 (4.7) | ||||
| 否 | 35 (94.6) | 41 (95.4) | ||||
| 同时服用精神药物或镇静催眠药(%) | 37 | 43 | 0.096 | 0.757 | ||
| 是 | 7 (18.9) | 7 (16.3) | ||||
| 否 | 30 (81.1) | 36 (83.7) | ||||
| 同时服用酒精(%) | 37 | 43 | 0.055 | 0.815 | ||
| 是 | 2 (5.4) | 4 (9.3) | ||||
| 否 | 35 (94.6) | 39 (90.7) | ||||
| 同时服用降糖药(%) | 37 | 43 | 0.130 | 0.719 | ||
| 是 | 1 (2.7) | 3 (7.0) | ||||
| 否 | 36 (97.3) | 40 (93.0) | ||||
| 同时服用其他物质(%) | 37 | 43 | 0.096 | 0.757 | ||
| 是 | 7 (18.9) | 7 (16.3) | ||||
| 否 | 30 (81.1) | 36 (83.7) | ||||
| 高血压病史(%) | 37 | 43 | 0.108 | 0.742 | ||
| 是 | 15 (40.5) | 19 (44.2) | ||||
| 否 | 22 (59.5) | 24 (55.8) | ||||
| 精神疾病史(%) | 37 | 43 | 0.571 | 0.450 | ||
| 是 | 10 (27.0) | 15 (34.9) | ||||
| 否 | 27 (73.0) | 28 (65.1) | ||||
| CKD病史(%) | 37 | 43 | 0.447 | 0.504 | ||
| 是 | 3 (8.1) | 1 (2.3) | ||||
| 否 | 34 (91.9) | 42 (97.7) | ||||
| 心率(次/min) | 35 | 82 (61, 110) | 28 | 95 (74, 112) | -0.478 | 0.633 |
| 收缩压(mmHg) | 36 | 81.8±20.5 | 32 | 76.1±20.2 | 1.155 | 0.252 |
| 注:n1为非难治性休克组参与分析的例数,n2为难治性休克组参与分析的例数;ACEI为血管紧张素转换酶抑制剂,ARB为血管紧张素受体阻滞剂,CKD为慢性肾脏病;1 mmHg=0.133 kPa | ||||||
| 项目 | n1 | 非难治性休克(n=37) | n2 | 难治性休克(n=43) | 统计值 | P值 |
| 血管活性药物或正性肌力药物种类 | 37 | 2 (1, 3) | 43 | 3 (2, 4) | -4.165 | <0.001 |
| 是否使用亚甲蓝(%) | 37 | 43 | 7.823 | 0.005 | ||
| 是 | 0 (0) | 10 (23.3) | ||||
| 否 | 37 (100) | 33 (76.7) | ||||
| 是否气管插管(%) | 37 | 43 | 4.606 | 0.032 | ||
| 是 | 18 (48.7) | 31 (72.1) | ||||
| 否 | 19 (51.4) | 12 (27.9) | ||||
| 是否心肺复苏(%) | 37 | 43 | 5.721 | 0.017 | ||
| 是 | 0 (0) | 8 (18.6) | ||||
| 否 | 37 (100) | 35 (81.4) | ||||
| 是否使用ECMO(%) | 37 | 43 | 10.974 | 0.001 | ||
| 是 | 0 (0) | 11 (25.6) | ||||
| 否 | 37 (100) | 32 (74.4) | ||||
| 是否使用血液净化(%) | 37 | 43 | 20.122 | <0.001 | ||
| 是 | 5 (13.5) | 27 (62.8) | ||||
| 否 | 32 (86.5) | 16 (37.2) | ||||
| 临床结局(%) | 37 | 43 | 4.49 | 0.034 | ||
| 存活 | 36 (97.3) | 34 (79.1) | ||||
| 死亡 | 1 (2.7) | 9 (20.9) | ||||
| 注:n1为非难治性休克组参与分析的例数,n2为难治性休克组参与分析的例数;非难治性休克组死亡病例是死于中毒治疗完成后继发的脓毒症及其诱发的多器官功能障碍综合征;ECMO为体外膜肺氧合 | ||||||
分析来诊的基本资料包括性别、年龄、服药剂量、服药至就诊间隔时间、共服物质、既往疾病、来诊生命体征,结果显示两组之间性别、服药剂量差异具有统计学意义,见表 2。
2.2.2 休克严重程度的相关因素的Logistic回归分析多因素分析,将性别、年龄、剂量、是否混合中毒进行二元Logistic回归分析,结果显示剂量是休克严重程度的独立影响因素,见表 4。
| 项目 | B | SE | Z | P值 | OR (95%CI) |
| 性别 | -0.769 | 0.575 | -1.338 | 0.181 | 0.46(0.15~1.43) |
| 年龄 | 0.012 | 0.015 | 0.793 | 0.428 | 1.01(0.98~1.04) |
| 剂量(每100 mg) | 0.360 | 0.127 | 2.825 | 0.005 | 1.43(1.12~1.84) |
| 是否混合中毒 | 0.393 | 0.557 | 0.706 | 0.480 | 1.48(0.5~4.41) |
为排除药物间的协同作用,进一步进行亚组分析,将仅服用氨氯地平未同服其他药物而中毒的非难治性休克和难治性休克的两组患者进行比较,服药剂量差异有统计学意义,见表 5。
| 项目 | 非难治性休克(n=19) | 难治性休克(n=15) | 统计值 | P值 |
| 性别(%) | - | 0.139 | ||
| 男 | 3 (15.8) | 6 (40.0) | ||
| 女 | 16 (84.2) | 9 (60.0) | ||
| 年龄 | 28.0 (23.0, 38.0) | 29.0 (23.5, 49.0) | -0.226 | 0.821 |
| 服药剂量(mg) | 250 (150, 350) | 450 (400, 650) | -2.923 | 0.003 |
| 服药至就诊间隔时间(h) | 6.0 (4.0, 11.0) | 10.2 (5.5, 12.0) | -0.706 | 0.480 |
| 高血压病史(%) | - | 0.718 | ||
| 是 | 5 (26.3) | 5 (33.3) | ||
| 否 | 14 (73.7) | 10 (66.7) | ||
| 精神疾病史(%) | - | 0.139 | ||
| 是 | 3 (15.8) | 6 (40.0) | ||
| 否 | 16 (84.2) | 9 (60.0) | ||
| CRF病史(%) | - | 1.000 | ||
| 是 | 2 (10.5) | 1 (6.7) | ||
| 否 | 17 (89.5) | 14 (93.3) | ||
| 心率(次/min) | 107 (83, 120) | 99 (78, 116) | 0.466 | 0.641 |
| 收缩压(mmHg)a | 77.0±15.5 | 73.0±22.2 | 0.602 | 0.552 |
| 注:a为(x±s);CRF为慢性肾功能衰竭 | ||||
用ROC曲线对中毒剂量和难治性休克进行分析,用氨氯地平中毒剂量预测难治性休克的ROC曲线下面积(AUC)为0.723(95%CI: 0.613~0.833)。最佳界值剂量为347.5 mg,敏感度0.651、特异度0.784。见图 1。
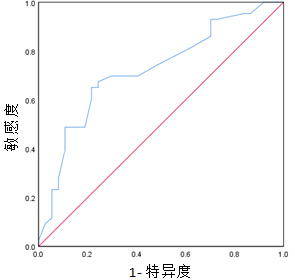
|
| 图 1 全部氨氯地平中毒患者中毒剂量预测难治性休克的ROC曲线 Fig 1 The ROC curve for predicting refractory shock in all patients with amlodipine poisoning |
|
|
纳入患者中有混合中毒病例,同服的药物特别是其他种类降压药物可能影响结果。仅氨氯地平中毒患者剂量和难治性休克的ROC曲线分析显示,AUC为0.795(95%CI: 0.634~0.956),最佳界值剂量为350 mg,敏感度0.867,特异度0.737。见图 2。
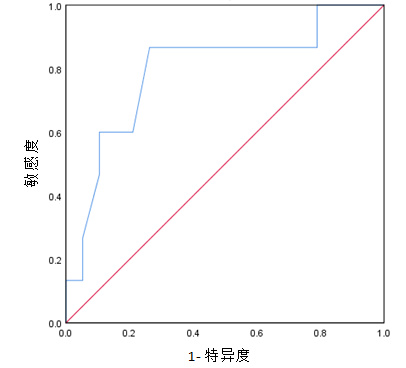
|
| 图 2 仅氨氯地平中毒患者中毒剂量预测难治性休克的ROC曲线 Fig 2 The ROC curve for predicting refractory shock in patients with amlodipine poisoning alone. |
|
|
服药剂量和难治性休克发生率的剂量反应关系表显示随着剂量的增大,发生难治性休克的比例也随之增加。具体见表 6。
| 剂量(mg) | 难治性休克比例 |
| 0~100 | 25.0% |
| 100~200 | 36.4% |
| 200~300 | 33.3% |
| 300~400 | 60.0% |
| 400~500 | 78.6% |
| ≥500 | 78.9% |
氨氯地平是一种二氢吡啶类钙通道阻滞剂,蛋白结合率98%,分布容积大(20~25 L/kg), 达峰时间6~12 h,作用时间长,半衰期约为32~45 h[76]。成人标准剂量为5~10 mg/d,一次给药,在临床上广泛应用。超量使用的主要毒性作用是休克,这主要是由于外周血管舒张引起的血管麻痹性休克,随后发生组织缺血、多器官功能障碍和乳酸酸中毒。氨氯地平中毒引起的心血管毒性与其药理作用有关,除了阻断外周血管L型钙通道之外,还通过一氧化氮途径降低血压[77-78]。动物实验也显示,大剂量氨氯地平中毒可引起心肌的负性肌力作用[77]。严重中毒时,休克表现为难治性休克甚至心脏骤停。非心源性肺水肿是CCBs过量的一种相对罕见的并发症,但在一些病例报告中已有记载。其机制尚不完全清楚,但被认为可能是由于肺毛细血管前血管舒张引起的肺血流量增加,导致肺跨毛细血管梯度和渗漏增加[8]。
氨氯地平的既往研究显示在健康男性志愿者口服氨氯地平2.5 mg、5 mg和10 mg后,剂量与血药浓度-时间曲线下面积(AUC)和血药浓度峰(Cmax)呈线性关系[79]。在氨氯地平治疗剂量的相关的临床研究中,氨氯地平在降压和治疗心绞痛方面均表现出较为显著的剂量依赖性作用[80-82]。然而,到目前为止,并无成人氨氯地平中毒的剂量与临床表现和严重程度的相关研究。
本研究选取本院曾诊治的氨氯地平中毒病例资料和检索近25年来发表的中毒病例资料进行回顾性研究,探讨服药剂量和休克严重程度的关系。对中毒后表现为非难治性休克和难治性休克的两组患者进行了比较。结果在分析了来诊的基本资料包括性别、年龄、服药剂量、服药至就诊间隔时间、共服物质、既往疾病、来诊生命体征后发现非难治性休克和难治性休克的两组之间性别和服药剂量具有统计学意义。随后进行的二元Logistic回归分析结果显示仅剂量是两组间的独立影响因素。与此同时,笔者对单纯氨氯地平中毒患者进行了非难治性休克和难治性休克的两组之间的亚组分析,也得出同样结果。这些结果可能提示药物剂量是中毒所致休克及其严重程度的重要相关因素。既往一项研究根据美国中毒中心数据对摄入不同氨氯地平剂量的<6岁的儿童数据进行了分析,分析了在四个剂量区间(<2.5 mg, 2.5~5.0 mg, 5.1~10.0 mg和>10 mg)所发生的临床中毒反应的风险。结果产生临床重要反应的最小剂量为2.5 mg(0.15 mg/kg), 而摄入>10 mg的儿童发生重要临床中毒反应的可能性是摄入≤5 mg的儿童的4.4倍[83]。提示随着药物剂量的增加,中毒风险随之增大。然而,此研究非成人患者数据。本研究是首次根据临床资料对成人氨氯地平中毒的药物剂量与休克的严重程度相关性进行研究,发现随着剂量的增大,发生难治性休克的比例也随之增加。
进一步笔者列出了剂量反应关系表,用受试者工作曲线对中毒剂量和难治性休克进行分析,结果最佳界值剂量为347.5 mg,此界值时显示了较好的敏感度(0.651)和特异度(0.784)。为了排除共服药物的影响,对仅氨氯地平中毒病例进行分析,得出的最佳界值剂量为350 mg,敏感度为0.867,特异性为0.737。提示临床在氨氯地平中毒剂量大于347.5 mg情况时,要对疾病严重程度给予高度重视,需要调配更多医疗资源,因为此时难治性休克概率大幅升高。对比两组的治疗可以看出难治性休克患者使用更多种类的血管活性药物,更多需要气管插管机械通气、血液净化治疗甚至ECMO等器官辅助支持治疗手段,更有可能发生心脏骤停,具有更高的病死率。剂量作为可以在第一时间掌握的临床数据信息,在本研究中显示出与疾病严重程度有较高的相关性,能更早期的帮助临床预测危重患者的可能性,及早给予更密切关注并做出更合理的临床决策。
笔者的研究是回顾性分析,多数病例资料缺少体重数据,因此不能对中毒剂量进行体重的标化,这可能影响了对个体剂量的精确评估,但笔者认为目前得到的非标化的药物剂量仍对临床有重要的指导意义。本研究的病例报道多为治疗成功的报告,导致样本病死率偏低,可能存在发表偏倚,难以进行与死亡相关的临床分析。但到目前为止,还没有大规模氨氯地平中毒的注册数据研究,笔者的研究为氨氯地平中毒的临床诊疗决策可能提供一定的参考。
综上所述,在因超量服用氨氯地平引起中毒的成人患者中,药物剂量与休克的严重程度相关,当剂量大于347.5 mg时要高度警惕难治性休克的发生,给予更多临床关注,调配更多医疗资源。
利益冲突 所有作者声明无利益冲突
作者贡献声明 李辉:论文撰写;张华:统计学分析;付源伟:数据收集及整理;郭治国、马青变:指导并审阅论文
| [1] | Vandroux D, Aujoulat T, Gaüzère BA, et al. Predicting factors for the need of extracorporeal membrane oxygenation for suicide attempts by cardiac medication: a single-center cohort study[J]. World J Emerg Med, 2022, 13(4): 283-289. DOI:10.5847/wjem.j.1920-8642.2022.070 |
| [2] | Gummin DD, Mowry JB, Spyker DA, et al. 2018 annual report of the American association of poison control centers' national poison data system (NPDS): 36th annual report[J]. Clin Toxicol (Phila), 2019, 57(12): 1220-1413. DOI:10.1080/15563650.2019.1677022 |
| [3] | Gummin DD, Mowry JB, Beuhler MC, et al. 2019 annual report of the American association of poison control centers' national poison data system (NPDS): 37th annual report[J]. Clin Toxicol (Phila), 2020, 58(12): 1360-1541. DOI:10.1080/15563650.2020.1834219 |
| [4] | St-Onge M, Anseeuw K, Cantrell FL, et al. Experts consensus recommendations for the management of calcium channel blocker poisoning in adults[J]. Crit Care Med, 2017, 45(3): e306-e315. DOI:10.1097/CCM.0000000000002087 |
| [5] | 蒋大明, 王兵侠, 谈定玉. 体外膜肺氧合救治重度氨氯地平中毒1例[J]. 中华急诊医学杂志, 2024, 33(3): 398-400. DOI:10.3760/cma.j.issn.1671-0282.2024.03.024 |
| [6] | Weiner L, Mazzeffi MA, Hines EQ, et al. Clinical utility of venoarterial-extracorporeal membrane oxygenation (VA-ECMO) in patients with drug-induced cardiogenic shock: a retrospective study of the Extracorporeal Life Support Organizations' ECMO case registry[J]. Clin Toxicol (Phila), 2020, 58(7): 705-710. DOI:10.1080/15563650.2019.1676896 |
| [7] | Beyls C, Malaquin S, Huette P, et al. Hemodynamic impact of molecular adsorbent recirculating system in refractory vasoplegic shock due to calcium channel blocker poisoning[J]. Int J Artif Organs, 2021, 44(12): 944-951. DOI:10.1177/03913988211007865 |
| [8] | Bringgold WR, Long MT. Amlodipine overdose complicated by non-cardiogenic pulmonary edema and diffuse alveolar hemorrhage: a case report[J]. Saudi J Anaesth, 2022, 16(1): 104-107. DOI:10.4103/sja.sja_388_21 |
| [9] | Patel T, Tietze D, Mehta AN. Amlodipine overdose[J]. Bayl Univ Med Cent Proc, 2013, 26(4): 410-411. DOI:10.1080/08998280.2013.11929022 |
| [10] | Tale S, Kumar M, Ghosh S, et al. A case of life-threatening amlodipine and atenolol overdose[J]. Indian J Crit Care Med, 2019, 23(6): 281-283. DOI:10.5005/jp-journals-10071-23181 |
| [11] | Matsushime S, Kuriyama A. Vasopressin for persistent hypotension due to amlodipine and olmesartan overdose: a case report[J]. Ann Med Surg (Lond), 2021, 65: 102292. DOI:10.1016/j.amsu.2021.102292 |
| [12] | Hedaiaty M, Eizadi-Mood N, Sabzghabaee AM. Noncardiogenic pulmonary edema after amlodipine overdose without refractory hypotension and bradycardia[J]. Case Rep Emerg Med, 2015, 2015: 546012. DOI:10.1155/2015/546012 |
| [13] | Reuter-Rice KE, Peterson BM. Conventional and unconventional lifesaving therapies in an adolescent with amlodipine ingestion[J]. Crit Care Nurse, 2016, 36(4): 64-69. DOI:10.4037/ccn2016524 |
| [14] | Koliastasis L, Lampadakis I, Milkas A, et al. Refractory shock from amlodipine overdose overcomed with hyperinsulinemia[J]. Cardiovasc Toxicol, 2022, 22(1): 63-66. DOI:10.1007/s12012-021-09699-2 |
| [15] | Hong IZ, Ng M, Sewa DW, et al. Use of extracorporeal membrane oxygenation in massive amlodipine overdose[J]. Arch Toxicol, 2022, 96(12): 3403-3405. DOI:10.1007/s00204-022-03364-5 |
| [16] | Meaney CJ, Sareh H, Hayes BD, et al. Intravenous lipid emulsion in the management of amlodipine overdose[J]. Hosp Pharm, 2013, 48(10): 848-854. DOI:10.1310/hpj4810-848 |
| [17] | Christina Gutierrez G, Dayton C, Attridge RL, et al. Angiotensin II use in treatment of refractory shock due to benazepril and amlodipine toxic ingestion[J]. J Pharm Pract, 2024, 37(2): 513-516. DOI:10.1177/08971900221137389 |
| [18] | Sandeep P, Ram R, Sowgandhi N, et al. Atenolol and amlodipine combination overdose managed with continuous venovenous hemodiafiltration: a case report[J]. Indian J Nephrol, 2014, 24(5): 327-329. DOI:10.4103/0971-4065.133033 |
| [19] | Nordmark Grass J, Ahlner J, Kugelberg FC, et al. A case of massive metoprolol and amlodipine overdose with blood concentrations and survival following extracorporeal corporeal membrane oxygenation (ECMO)[J]. Clin Toxicol (Phila), 2019, 57(1): 66-68. DOI:10.1080/15563650.2018.1491985 |
| [20] | Upreti V, Ratheesh VR, Dhull P, et al. Shock due to amlodipine overdose[J]. Indian J Crit Care Med, 2013, 17(6): 375-377. DOI:10.4103/0972-5229.123452 |
| [21] | Kumar S, Thakur D, Gupta RK, et al. Unresponsive shock due to amlodipine overdose: an unexpected cause[J]. J Cardiovasc Thorac Res, 2018, 10(4): 246-247. DOI:10.15171/jcvtr.2018.43 |
| [22] | Ebihara T, Morita M, Kawada M, et al. Efficacy of isoproterenol for treating amlodipine overdose resulting in bradycardia[J]. Acute Med Surg, 2017, 4(3): 353-357. DOI:10.1002/ams2.284 |
| [23] | Kute VB, Shah PR, Goplani KR, et al. Successful treatment of refractory hypotension, noncardiogenic pulmonary edema and acute kidney injury after an overdose of amlodipine[J]. Indian J Crit Care Med, 2011, 15(3): 182-184. DOI:10.4103/0972-5229.84901 |
| [24] | Chudow M, Ferguson K. A case of severe, refractory hypotension after amlodipine overdose[J]. Cardiovasc Toxicol, 2018, 18(2): 192-197. DOI:10.1007/s12012-017-9419-x |
| [25] | Karbek Akarca F, Akceylan E, Kıyan S. Treatment of amlodipine intoxication with intravenous lipid emulsion therapy: a case report and review of the literature[J]. Cardiovasc Toxicol, 2017, 17(4): 482-486. DOI:10.1007/s12012-017-9421-3 |
| [26] | Brunette-Lawrey E, Croft F. Losartan and amlodipine overdose-Case Report of a patient with anuric renal failure prior to the onset of hypotension[J]. N Z Med J, 2016, 129(1435): 84-86. |
| [27] | Nasa P, Singh A, Juneja D, et al. Continuous venovenous hemodiafiltration along with charcoal hemoperfusion for the management of life-threatening lercanidipine and amlodipine overdose[J]. Saudi J Kidney Dis Transpl, 2014, 25(6): 1255-1258. DOI:10.4103/1319-2442.144262 |
| [28] | Ando M, Nakasako S, Ariyoshi K, et al. Re-elevation of serum amlodipine level after lipid emulsion therapy in an overdose case[J]. J Clin Pharm Ther, 2019, 44(6): 970-973. DOI:10.1111/jcpt.13018 |
| [29] | Gérard L, Galloy AC, Capron A, et al. Mixed amlodipine/valsartan overdose treated by the molecular adsorbent recirculating system (MARSTM)[J]. Clin Toxicol (Phila), 2015, 53(6): 573-577. DOI:10.3109/15563650.2015.1050594 |
| [30] | Lai F, Zhang Y, Xie DP, et al. Successful treatment with integrated Chinese and western medicine for severe overdose of amlodipine: a case report[J]. Chin J Integr Med, 2015, 21(9): 703-706. DOI:10.1007/s11655-015-2130-5 |
| [31] | Ramanathan K, Mohanty B, Tang S, et al. Extracorporeal therapy for amlodipine poisoning[J]. J Artif Organs, 2020, 23(2): 183-186. DOI:10.1007/s10047-019-01132-4 |
| [32] | Weinberg RL, Bouchard NC, Abrams DC, et al. Venoarterial extracorporeal membrane oxygenation for the management of massive amlodipine overdose[J]. Perfusion, 2014, 29(1): 53-56. DOI:10.1177/0267659113498807 |
| [33] | Naha K, Suryanarayana J, Aziz RA, et al. Amlodipine poisoning revisited: Acidosis, acute kidney injury and acute respiratory distress syndrome[J]. Indian J Crit Care Med, 2014, 18(7): 467-469. DOI:10.4103/0972-5229.136078 |
| [34] | Ghosh S, Sircar M. Calcium channel blocker overdose: experience with amlodipine[J]. Indian J Crit Care Med, 2008, 12(4): 190-193. DOI:10.4103/0972-5229.45080 |
| [35] | Gautam S, Chamlagain M, Yadav GK, et al. Once was not enough: a case report of the concomitant intoxication of amlodipine (calcium channel blocker) and clonazepam (benzodiazepine)[J]. Clin Case Rep, 2022, 10(7): e6042. DOI:10.1002/ccr3.6042 |
| [36] | St-Onge M, Ajmo I, Poirier D, et al. L-Carnitine for the treatment of a calcium channel blocker and metformin poisoning[J]. J Med Toxicol, 2013, 9(3): 266-269. DOI:10.1007/s13181-013-0301-3 |
| [37] | Rizvi I, Ahmad A, Gupta A, et al. Life-threatening calcium channel blocker overdose and its management[J]. BMJ Case Rep, 2012, 2012: bcr0120125643. DOI:10.1136/bcr.01.2012.5643 |
| [38] | Plumb JOM, Stewart C, Eddleston M, et al. Prolonged refractory hypotension following combined amlodipine and losartan ingestion responsive to metaraminol[J]. Case Rep Med, 2011, 2011: 283672. DOI:10.1155/2011/283672 |
| [39] | Kao R, Landry Y, Chick G, et al. Bilateral blindness secondary to optic nerve ischemia from severe amlodipine overdose: a case report[J]. J Med Case Rep, 2017, 11(1): 211. DOI:10.1186/s13256-017-1374-4 |
| [40] | West PL, McKeown NJ, Hendrickson RG. Iatrogenic lipid emulsion overdose in a case of amlodipine poisoning[J]. Clin Toxicol (Phila), 2010, 48(4): 393-396. DOI:10.3109/15563651003670843 |
| [41] | Agarwal MA, Flatt D, Khouzam RN. The potential detrimental effects of calcium channel blockers' overdose and current available management[J]. Ann Transl Med, 2018, 6(1): 16. DOI:10.21037/atm.2018.01.03 |
| [42] | Harris NS. Case 24-2006: A 40-Year-Old Woman with Hypotension after an Overdose of Amlodipine[J]. N Engl J Med, 2006, 355(6): 602-611. DOI:10.1056/NEJMcpc069016 |
| [43] | Haughey R, Vernick W, Gutsche J, et al. Use of veno-venous extracorporeal membrane oxygenation to treat severe combined calcium channel blocker and angiotensin converting enzyme inhibitor overdose[J]. Perfusion, 2019, 34(2): 167-169. DOI:10.1177/0267659118798181 |
| [44] | Sutar A, Venkategowda PM, Murthy A, et al. Severe amlodipine toxicity: a case rescued with extracorporeal membrane oxygenation[J]. Indian J Crit Care Med, 2020, 24(5): 365-366. DOI:10.5005/jp-journals-10071-23423 |
| [45] | Wood DM, Wright KD, Jones AL, et al. Metaraminol (Aramine) in the management of a significant amlodipine overdose[J]. Hum Exp Toxicol, 2005, 24(7): 377-381. DOI:10.1191/0960327105ht538oa |
| [46] | Jang DH, Nelson LS, Hoffman RS. Methylene blue in the treatment of refractory shock from an amlodipine overdose[J]. Ann Emerg Med, 2011, 58(6): 565-567. DOI:10.1016/j.annemergmed.2011.02.025 |
| [47] | Beavers JR, Stollings JL, Rice TW. Hyponatremia induced by hyperinsulinemia-euglycemia therapy[J]. Am J Health Syst Pharm, 2017, 74(14): 1062-1066. DOI:10.2146/ajhp160262 |
| [48] | Adams BD, Browne WT. Amlodipine overdose causes prolonged calcium channel blocker toxicity[J]. Am J Emerg Med, 1998, 16(5): 527-528. DOI:10.1016/s0735-6757(98)90011-0 |
| [49] | Hopkins LE, Sunkersing J, Jacques A. Too many pills to swallow: a case of a mixed overdose[J]. J Intensive Care Soc, 2017, 18(3): 247-250. DOI:10.1177/1751143717693860 |
| [50] | Rasmussen L, Husted SE, Johnsen SP. Severe intoxication after an intentional overdose of amlodipine[J]. Acta Anaesthesiol Scand, 2003, 47(8): 1038-1040. DOI:10.1034/j.1399-6576.2003.00181.x |
| [51] | Zahed NS, Hassanian-Moghaddam H, Zamani N. A fatal case of amlodipine toxicity following iatrogenic hypercalcemia[J]. Cardiovasc Toxicol, 2018, 18(3): 290-293. DOI:10.1007/s12012-018-9445-3 |
| [52] | Hung YM, Olson KR. Acute amlodipine overdose treated by high dose intravenous calcium in a patient with severe renal insufficiency[J]. Clin Toxicol (Phila), 2007, 45(3): 301-303. DOI:10.1080/15563650601072233 |
| [53] | El Houari T, Haddiya I, El Ouafi N, et al. A survival case in a severe amlodipine intoxication[J]. Case Rep Cardiol, 2013, 2013: 842606. DOI:10.1155/2013/842606 |
| [54] | Essink J, Berg S, Montange J, et al. Single-pass albumin dialysis as rescue therapy for pediatric calcium channel blocker overdose[J]. J Investig Med High Impact Case Rep, 2022, 10: 23247096221105251. DOI:10.1177/23247096221105251 |
| [55] | Osman AF, Prasad RM, Marein S, et al. Multi-organ dysfunction as a presentation of calcium channel blocker intoxication[J]. BMJ Case Rep, 2022, 15(1): e245711. DOI:10.1136/bcr-2021-245711 |
| [56] | Azendour H, Belyamani L, Atmani M, et al. Severe amlodipine intoxication treated by hyperinsulinemia euglycemia therapy[J]. J Emerg Med, 2010, 38(1): 33-35. DOI:10.1016/j.jemermed.2007.11.077 |
| [57] | Vogt S, Mehlig A, Hunziker P, et al. Survival of severe amlodipine intoxication due to medical intensive care[J]. Forensic Sci Int, 2006, 161(2/3): 216-220. DOI:10.1016/j.forsciint.2006.02.051 |
| [58] | Connor-Schuler RL, Carr JM, Reaven MS, et al. The efficacy of albumin dialysis in the reversal of refractory vasoplegic shock due to amlodipine toxicity[J]. Crit Care Explor, 2020, 2(6): e0120. DOI:10.1097/CCE.0000000000000120 |
| [59] | Hasson R, Mulcahy V, Tahir H. Amlodipine poisioning complicated with acute non-cardiogenic pulmonary oedema[J]. BMJ Case Rep, 2011, 2011: bcr0720114467. DOI:10.1136/bcr.07.2011.4467 |
| [60] | Garg SK, Goyal PK, Kumar R, et al. Management of life-threatening calcium channel blocker overdose with continuous veno-venous hemodiafiltration with charcoal hemoperfusion[J]. Indian J Crit Care Med, 2014, 18(6): 399-401. DOI:10.4103/0972-5229.133939 |
| [61] | Khan S, Norville KJ, Khan I, et al. Calcium channel blocker overdose treated with calcium resulting in pancreatitis: a case report[J]. Cureus, 2019, 11(4): e4493. DOI:10.7759/cureus.4493 |
| [62] | Ezidiegwu C, Spektor Z, Nasr MR, et al. A case report on the role of plasma exchange in the management of a massive amlodipine besylate intoxication[J]. Ther Apher Dial, 2008, 12(2): 180-184. DOI:10.1111/j.1744-9987.2008.00567.x |
| [63] | Laes JR, Williams DM, Cole JB. Improvement in hemodynamics after methylene blue administration in drug-induced vasodilatory shock: a case report[J]. J Med Toxicol, 2015, 11(4): 460-463. DOI:10.1007/s13181-015-0500-1 |
| [64] | Varpula T, Rapola J, Sallisalmi M, et al. Treatment of serious calcium channel blocker overdose with levosimendan, a calcium sensitizer[J]. Anesth Analg, 2009, 108(3): 790-792. DOI:10.1213/ane.0b013e3181931737 |
| [65] | Jović-Stosić J, Putić V, Zivanović D, et al. Failure of intravenous lipid emulsion in treatment of cardiotoxicity caused by mixed overdose including dihydropyridine calcium channel blockers[J]. Vojnosanit Pregl, 2016, 73(1): 88-91. DOI:10.2298/vsp141216018j |
| [66] | Kanagarajan K, Marraffa JM, Bouchard NC, et al. The use of vasopressin in the setting of recalcitrant hypotension due to calcium channel blocker overdose[J]. Clin Toxicol (Phila), 2007, 45(1): 56-59. DOI:10.1080/15563650600795669 |
| [67] | Shetty K, Sherif L, Babu R, et al. Noninvasive ventilation in a patient with noncardiogenic pulmonary edema following amlodipine poisoning[J]. J Anaesthesiol Clin Pharmacol, 2015, 31(2): 264-266. DOI:10.4103/0970-9185.155205 |
| [68] | Wilffert B, Boskma RJ, van der Voort PJ, et al. 4-Aminopyridine (fampridine) effectively treats amlodipine poisoning: a case report[J]. J Clin Pharm Ther, 2007, 32(6): 655-657. DOI:10.1111/j.1365-2710.2007.00861.x |
| [69] | Koch AR, Vogelaers DP, Decruyenaere JM, et al. Fatal intoxication with amlodipine[J]. J Toxicol Clin Toxicol, 1995, 33(3): 253-256. DOI:10.3109/15563659509017993 |
| [70] | Miranda CH, Xavier L, Fiorante F, et al. Cardiac rhythm disturbances associated with amlodipine acute intoxication[J]. Cardiovasc Toxicol, 2012, 12(4): 359-362. DOI:10.1007/s12012-012-9176-9 |
| [71] | Teker MG, Ozdemir H, Saidoglu L, et al. Levosimendan as a rescue adjunct in amlodipine intoxication: a case report[J]. Middle East J Anaesthesiol, 2010, 20(6): 869-872. |
| [72] | Raj A, Panda PK, Singh SS. Amlodipine (150 Mg) poisoning: a case study[J]. Curr Drug Saf, 2018, 13(2): 144-147. DOI:10.2174/1574886313666180313120659 |
| [73] | Boyer EW, Shannon M. Treatment of calcium-channel-blocker intoxication with insulin infusion[J]. N Engl J Med, 2001, 344(22): 1721-1722. DOI:10.1056/NEJM200105313442215 |
| [74] | Saravu K, Balasubramanian R. Near-fatal amlodipine poisoning[J]. J Assoc Physicians India, 2004, 52: 156-157. |
| [75] | Rafeq R, Salzman M. Use of concentrated insulin in the management of calcium channel blocker overdose: a case report[J]. J Pharm Pract, 2023, 36(6): 1519-1522. DOI:10.1177/08971900221116189 |
| [76] | Wong A, Hoffman RS, Walsh SJ, et al. Extracorporeal treatment for calcium channel blocker poisoning: systematic review and recommendations from the EXTRIP workgroup[J]. Clin Toxicol (Phila), 2021, 59(5): 361-375. DOI:10.1080/15563650.2020.1870123 |
| [77] | Zhang X, Hintze TH. Amlodipine releases nitric oxide from canine coronary microvessels: an unexpected mechanism of action of a calcium channel-blocking agent[J]. Circulation, 1998, 97(6): 576-580. DOI:10.1161/01.cir.97.6.576 |
| [78] | Cole JB, Lee SC, Prekker ME, et al. Vasodilation in patients with calcium channel blocker poisoning treated with high-dose insulin: a comparison of amlodipine versus non-dihydropyridines[J]. Clin Toxicol (Phila), 2022, 60(11): 1205-1213. DOI:10.1080/15563650.2022.2131565 |
| [79] | Williams DM, Cubeddu LX. Amlodipine pharmacokinetics in healthy volunteers[J]. J Clin Pharmacol, 1988, 28(11): 990-994. DOI:10.1002/j.1552-4604.1988.tb03119.x |
| [80] | Frick MH, McGibney D, Tyler HM. A dose-response study of amlodipine in mild to moderate hypertension[J]. J Intern Med, 1989, 225(2): 101-105. DOI:10.1111/j.1365-2796.1989.tb00047.x |
| [81] | Cocco G, Alfiero R. A double-blind dose-response study of amlodipine in patients with stable angina pectoris[J]. Eur Heart J, 1991, 12(2): 169-174. DOI:10.1093/oxfordjournals.eurheartj.a059864 |
| [82] | Mehta JL, Lopez LM, Vlachakis ND, et al. Double-blind evaluation of the dose-response relationship of amlodipine in essential hypertension[J]. Am Heart J, 1993, 125(6): 1704-1710. DOI:10.1016/0002-8703(93)90762-x |
| [83] | Benson BE, Spyker DA, Troutman WG, et al. Amlodipine toxicity in children less than 6 years of age: a dose-response analysis using national poison data system data[J]. J Emerg Med, 2010, 39(2): 186-193. DOI:10.1016/j.jemermed.2009.02.016 |
 2025, Vol. 34
2025, Vol. 34




